Struggling with joint pain during menopause?
You’re not alone — and it’s not in your head. Hormonal shifts can trigger inflammation, stiffness, and even long-term joint discomfort.
But science-backed supplements may help. From collagen peptides to curcumin, magnesium, and beyond — this guide breaks down the most effective natural solutions for menopause-related joint pain.
This short video outlines the benefits and science behind 5 Supplements That Help Joint Pain During Menopause.
Enjoyed watching? Keep reading to learn about what causes the hormonal changes and how to manage them!
What Causes Joint Pain During Menopause?
While supplements can offer relief, it’s important to first understand why joint pain becomes more common during menopause. A combination of hormonal changes, ageing processes, and shifts in body composition can all contribute to increased inflammation, reduced joint cushioning, and greater discomfort. Let’s take a closer look at the key factors involved
Hormonal Fluctuations and Their Effects
Estrogen plays a pivotal role in maintaining joint and cartilage health. Its decline during menopause leads to increased inflammation, diminished collagen synthesis, and reduced lubrication in joints. These factors contribute to joint pain and stiffness in the joints.
Aging and Joint Health
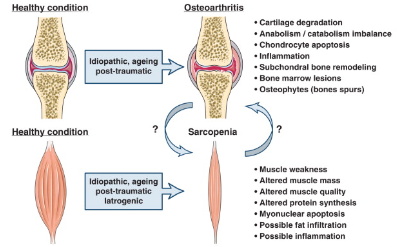
Aging further compounds joint-related challenges. Reduced muscle mass and strength, known as sarcopenia, often accompany menopause, destabilizing joints and increasing susceptibility to injury.
Moreover, the cushioning in joints begins to thin, and the fluid that keeps your joints lubricated may decrease. Combined with the hormonal changes of menopause, this can make joint pain more noticeable, especially in areas like the knees and hips.
Weight Gain and Its Impact on Joints
Weight gain, which is common during menopause, places additional mechanical stress on weight-bearing joints.
In cases of extreme weight gain, like obesity, the physical burden increases. This also leads to systemic inflammation. This happens because fat tissue releases tiny signaling proteins called pro-inflammatory cytokines.
These cytokines act as messengers, signaling the body to initiate an inflammatory response. While inflammation helps the body heal, too many cytokines over time can cause ongoing inflammation, which worsens joint pain and damages cartilage.
Decreased Muscle Mass and Joint Pain
During menopause, there is a notable loss of both muscle mass and bone mass, primarily due to the decline in estrogen levels. This loss can reduce joint stability, leaving them more vulnerable to wear and tear. Research underscores the importance of maintaining lean muscle to support joint function and alleviate pain.
Symptoms of Menopausal Joint Pain
Menopausal joint pain typically manifests as stiffness, swelling, and reduced range of motion, particularly in the morning or after prolonged inactivity. Commonly affected areas include the knees, hips, hands, and lower back. These aches and pains can vary in intensity, often worsening with weight gain, inactivity, or underlying inflammatory conditions like osteoarthritis, a condition where bones become brittle and prone to fractures.
What Makes Menopausal Joint Pain Worse?
Symptoms such as hot flashes, sleep disturbances, and mood changes indirectly intensify joint discomfort. When estrogen levels drop, it disrupts the part of the brain responsible for regulating body temperature. Here’s how they interact.
Hot Flashes, Sleep Disturbances, and Inflammation
When estrogen levels drop, it disrupts the part of the brain responsible for regulating body temperature.
This leads to rapid dilation of blood vessels, causing sudden heat surges (hot flashes) and night sweats that disturb sleep patterns.
Poor sleep elevates cortisol — the body’s primary stress hormone — which drives up systemic inflammation and breaks down collagen, a key structural protein supporting joints.
The combined effects of inflammation and cortisol slow the body’s natural healing processes, making joints more vulnerable to damage and pain.
Mood Changes, Hormones, and Joint Pain
Mood swings are another common symptom during menopause, largely driven by fluctuations in estrogen and progesterone levels.
These hormonal changes influence neurotransmitters like serotonin, which not only regulate mood but also impact inflammation pathways.
A disrupted emotional state can, therefore, further amplify inflammatory processes that affect joint health.
The Gut–Brain Axis: Gut Health Influences Inflammation
Emerging evidence highlights the strong connection between gut health, serotonin production, and systemic inflammation.
Since a significant proportion of the body’s serotonin is produced in the gut, maintaining a healthy gut microbiome can help regulate mood and support lower inflammation levels — indirectly benefiting joint comfort.
Learn more about serotonin and how gut health can impact its production in our Gut-Brain Axis article.
Natural Ways to Manage Menopausal Joint Pain
To nurture your joints and promote overall well-being during menopause, consider incorporating these scientifically supported supplements and nutrients into your daily routine.
Best Supplements for Menopause Joint Pain Relief
- Glucosamine and Chondroitin Sulfate: These supplements provide the body with the building blocks to maintain healthy cartilage and joint fluid, helping to reduce menopause joint pain and inflammation and improve joint mobility.
- Collagen Peptides: Collagen is the main protein in connective tissues, including cartilage. Collagen peptides, such as hydrolyzed bovine collagen powder, can support menopausal women. They promote muscle growth and improve muscle mass. Moreover, collagen can reduce inflammation—key factors in managing joint pain during menopause.
- Nano Curcumin: Curcumin, the active compound in turmeric, is known for its potent anti-inflammatory and antioxidant properties. Nano-curcumin, a highly absorbable form, enhances delivery to reduce inflammation and pain effectively.
- Vitamin D: Crucial for calcium absorption and overall bone health. Inadequate levels of vitamin D can lead to weaker bones and may contribute to joint pain. Supplementing with vitamin D may improve symptoms by reducing bone loss in postmenopausal women.
- Calcium: Essential for maintaining bone strength and preventing osteoporosis. During menopause, calcium supplementation can help offset bone density loss caused by declining estrogen levels.
- Magnesium: This mineral supports muscle relaxation and nerve function, which can indirectly reduce joint stiffness and pain. Magnesium also helps maintain strong bones by supporting calcium absorption. Studies suggest magnesium supplementation can enhance vitamin D levels.
You can learn more about the collagen’s impact on overall health in our dedicated article .
Support Your Joints Through Menopause: Our advanced Collagen Joint Health blend combines the power of hydrolyzed bovine collagen and nano-curcumin, as discussed in this guide, with essential minerals for enhanced joint health. Get exclusive early access and a 25% discount upon release!

Dietary Considerations
- Anti-inflammatory and Antioxidant Foods: Foods such as berries, vegetables and leafy greens, nuts, seeds, and herbs contain anti-inflammatory and antioxidant compounds that combat inflammation and oxidative stress. A diet rich in these foods can help manage inflammation, protect cells from damage, and support the body’s natural defense mechanisms.
- Whole Grains: Foods such as brown rice and oats, are excellent sources of fiber and other nutrients. Fiber helps regulate blood sugar levels, promotes healthy digestion, and supports weight management, easing stress on joints. Fiber also promotes a healthy gut microbiome, which plays a crucial role in managing inflammation.
- Omega-3 Fatty Acids: Found in sources like fish oil, flaxseed, and walnuts, omega-3s are renowned for their anti-inflammatory properties. Some studies indicate that combining omega-3 fatty acids with glucosamine may provide further pain relief and improve joint function.
Lifestyle Changes to Manage Joint Pain
- Exercise and Joint Health: Regular, low-impact exercises such as swimming, yoga, and walking enhance joint mobility and reduce stiffness. Resistance training strengthens surrounding muscles, providing additional support to joints.
- Maintaining a Healthy Weight: Weight management reduces mechanical stress on joints and mitigates systemic inflammation. Combining a balanced diet with regular physical activity is key to achieving and sustaining a healthy weight.
- Stress Management Techniques: Mindfulness practices, such as meditation and deep breathing, lower cortisol levels. This can reduce inflammation and improve pain perception. These practices also enhance overall mental well-being, which is closely linked to physical health.

Next Steps: Choosing the Right Supplement for You
Menopause presents unique challenges to joint health, but it also offers an opportunity to embrace a new narrative of vitality. By understanding the interplay of hormones, lifestyle, and nutrition, women can take proactive steps to support mobility, comfort, enduring radiance and quality of life during this transformative phase. This holistic approach aligns with the Japanese concept of Konenki (更年期), emphasizing balance and resilience during menopause.

Frequently Asked Questions (FAQs)
Hormonal changes, particularly the decline in oestrogen, can increase inflammation and reduce collagen production. This leads to joint stiffness, discomfort, and decreased flexibility — especially in the knees, hips, and lower back.
Results vary, but many women report noticeable improvement in joint flexibility and reduced pain within 4 to 12 weeks of consistent use. Collagen and curcumin may take longer for full effects as they build up in the body over time.
There’s no one-size-fits-all answer. However, hydrolysed collagen, curcumin (especially nano-formulated), magnesium, and vitamin D are often recommended together for a holistic anti-inflammatory and joint-supportive effect.
Absolutely. In addition to supplements, regular low-impact exercise (like swimming or yoga), a nutrient-rich anti-inflammatory diet, stress reduction, and maintaining a healthy weight are essential for joint relief during menopause.
Join Us in Redefining Beauty
Subscribe for Exclusive Insights